Everyday 17 Veterans Commit Suicide
- GJD
- Nov 10, 2023
- 5 min read
Updated: Nov 10, 2024

Introduction
Two days ago, I lost a MILITARY brother to suicide. He leaves behind a wife and several school-age children. My community mourns his loss and remembers all those before him.
It is no secret that veterans are at a higher risk of committing suicide than the general population. In fact, according to a report by the Department of Veterans Affairs (VA), everyday, 17 veterans take their own lives. This heartbreaking figure has been the center of attention for years. Why - despite the numerous programs and facilities addressing this issue - do veterans still find it challenging to reach out for help? I’d like to discuss this using four major headings.
UNDERLYING TRAUMA AND PTSD. ONCE YOU SEE IT, YOU OWN IT! YOU CAN’T “JUST GET OVER IT!”
Many veterans suffer from underlying PTSD and trauma, which can be a trigger for suicidal thoughts and actions. These trauma experiences can come from a variety of sources, including combat, sexual assault, and military sexual trauma. Veterans dealing with PTSD may find it challenging to express themselves and may even avoid seeking help often because of this.
This couldn't be truer. *Please forgive the graphic nature of the following.* How do you talk about a child who was burned to death or had his leg blown off or the older man who was handing out food when a snipper gut shot him, and he was dead 20 minutes later. How do you talk about the headshot that left a patient breathing but otherwise deceased. Or even the tortured prisoners you were asked to care for. No one gets it, nor do they want to hear it. For me, that was my daily reality – my memories.
On return, how do I reconcile this and resume everyday life when the news is filled with so much of the same. Not in one area but in many. Especially when no one wants to hear my story. Why would they?
STIGMA AND SHAME. LET THE VETERAN BE HUMAN! THERE IS NO SHAME IN BEING HUMAN! IT IS BETTER TO SAY NOTHING THEN TO BE CALLOUS.
One of the biggest hurdles that keep veterans from seeking help is the social stigma and shame attached to mental illness. This is particularly significant in the military culture, where seeking help for mental health issues is often viewed as a sign of weakness and vulnerability. Such stereotypes make it difficult for veterans to talk about their struggles without feeling the weight of judgment and disapproval from their peers.
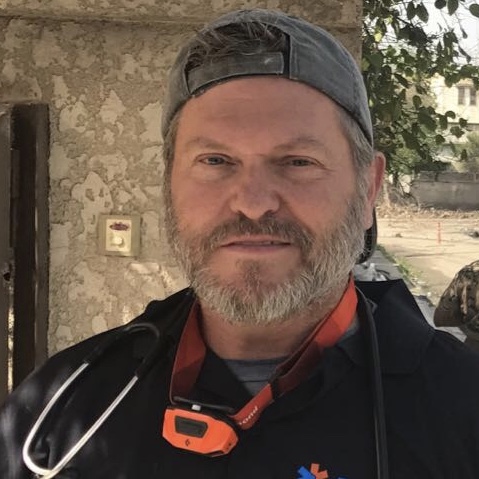
I have personally experienced this. My military and civilian work prepared me and led me into front-line combat, where I saw terrible atrocities on children, women, old men, soldiers, and the 'enemy.' Most recently (in 2017), I provided front-line medical care in Mosul, Iraq, during its liberation from ISIS (several trips). Unfortunately, some of these visions recur daily. On my return, I tried to talk about the pain, discovering one of three responses.
1. The listener said, "You volunteered."
2. The listener said, "Get over it."
3. The listener's eyes turned me off, and they didn't know what to say or do and couldn't wait until I was done.
As a result, I gravitated to silence and suffered alone. Over time, I was spiraling into a deeper state of depression (PTSD).
THE READJUSTMENT PROCESS. A VETERAN NEEDS SOMEON WHO CAN HELP THEM REASSIMILATE. WE ALL NEED A FRIEND WHO IS WILLING TO LISTEN!
Life after service can be overwhelming for veterans, and the readjustment process can take years. Many veterans experience a feeling of isolation, disorientation, and a lack of purpose once they leave the military. These emotions can lead to depression, anxiety, and trauma that may be hard to deal with. This lack of direction and a sense of community can make it harder for veterans to seek help, as they may believe that no one understands what they are going through.
For me, I live in remote regions with no structured support. Trying to reassimilate seemed a lonely journey. My friends lived far away, and my community had no concept of what I needed. This led me to isolate more and the more I isolated, the less support I had. (see "stigma and shame")
HEALTHCARE ACCESS. A VETERAN DESERVES TO FIND HAPPINESS AGAIN. THERE IS NO SHAME IN COUNSELING. FIND A FIT AND PROCESS YOUR PAIN.
While the VA has made significant strides in improving healthcare for veterans, there are still gaps in the healthcare system that keep veterans from accessing help. Long wait times, understaffed facilities, and a lack of mental health providers are some of the reasons veterans may not receive the care they need. Mental healthcare is also not always covered by insurance, which can make it cost-prohibitive for some veterans.
I reached out to the VA, and on my first visit, the psychologist told me to listen to the Eagle's song, "Take it easy." I was suicidal, and no follow-up was scheduled. It was apparent he had no experience in this arena, and I left feeling more alone than when I had arrived. I also refused to seek help again for a long time. I thought it was worthless. Sometime later, I tried again. This time, I saw a clinician who performed 'eye movement desensitization and reprocessing" (EMDR), which was supposed to help me overcome my visions. Sadly, when doing this, I could see her texting, not paying attention to me. I felt like a number in her calendar and stopped going. I also didn't feel it helped. I hear it helps some people. The bottom line is that inexperienced clinicians may not have sufficient training on military culture and the unique emotional and psychological stressors veterans face. This can make it hard to open up and receive the right help.
After years of suffering, help finally came when I saw an old vet psychiatrist for a four-hour intake meeting. He validated my issues, and we met regularly for several years. He cared, called me between appointments, and even emailed me, ensuring I was okay. Unfortunately, he was a fee for service provider at $200/hour. Most veterans cannot afford this.
For me, therapy with someone who truly understand my situation was critical. With that said, if you have PTSD, don't wait for the common link. Most therapists provide good tools that may be the difference between suicide or not. See someone. Please see someone.
Conclusion
I could ramble in this post, but I have said enough. I am sad as I feel the loss of another veteran, and I fear for the pain his family will now face. For me, I have three former SERE friends who check in on me regularly. They knew I had been in the s=*t, recognized my pain, and reached out on a regular basis. It has made a big difference. They listen to me and tell me they are here if I need them.
If you have a veteran in your life, listen to their words. Their reality may be hidden. Touch their arm and let them know you are listening and are here if they need you. Check in on them.
For more information on veteran suicide assistance (service is for the veteran and loved ones), go to https://www.veteranscrisisline.net
Anxiety VA Disability – veteransguide.org/va-disability/ratings/anxiety-disorders/
VA Disability Appeals – veteransguide.org/va-disability/appeals/


Comments